Pancreatic mucinous cystic neoplasm is a term that might sound intimidating, but it’s essential to understand what it entails for those affected by it. This type of cystic tumor primarily affects the pancreas and is predominantly found in women. The pancreas, a vital organ located behind the stomach, plays a crucial role in digestion and regulating blood sugar levels. Pancreatic mucinous cystic neoplasms are classified as premalignant or malignant tumors, meaning they have the potential to develop into pancreatic cancer if left untreated. Early detection and management are key to preventing complications and ensuring a positive prognosis.
The prevalence of pancreatic mucinous cystic neoplasms has been on the rise, partly due to advancements in imaging technology that allow for earlier detection. While the exact cause remains unclear, researchers believe that genetic mutations and hormonal factors may contribute to their development. The symptoms associated with these cystic tumors can vary widely, from mild discomfort to severe abdominal pain, depending on their size and location within the pancreas. Awareness of the signs and symptoms is crucial for timely medical intervention.
As medical science continues to evolve, so does our understanding of pancreatic mucinous cystic neoplasms. With improved diagnostic tools and treatment options, patients have better chances of managing the condition effectively. This article aims to provide comprehensive insights into this condition, covering everything from its symptoms and diagnosis to the latest treatment approaches and lifestyle considerations. Whether you're a patient, caregiver, or healthcare professional, this guide will equip you with the knowledge needed to make informed decisions about pancreatic mucinous cystic neoplasms.
Read also:Deliciously Easy How Do You Cook Little Smokies On The Stove For A Flavorful Treat
What Is Pancreatic Mucinous Cystic Neoplasm?
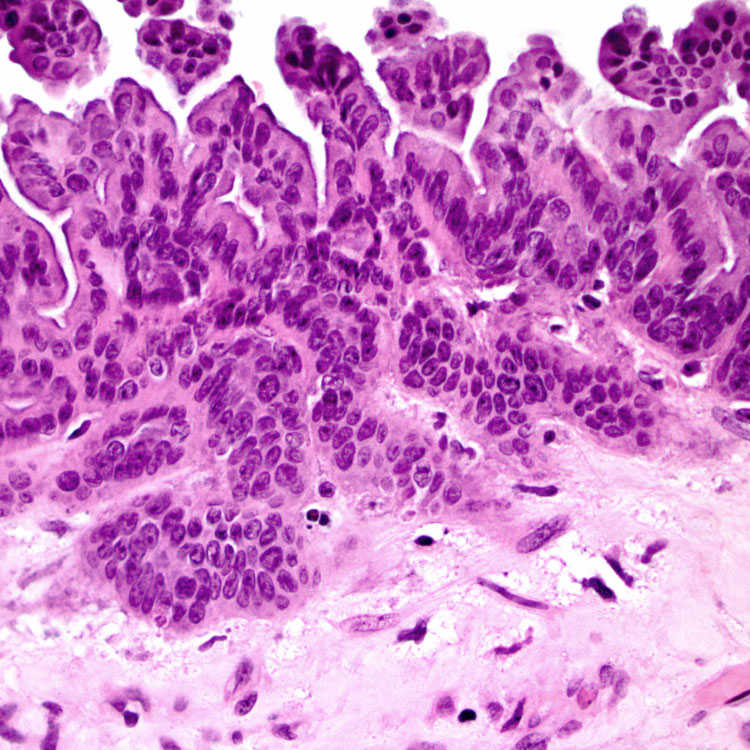
Pancreatic mucinous cystic neoplasm refers to a specific type of cystic tumor that develops in the pancreas. Unlike nonmucinous cysts, these neoplasms produce mucin, a jelly-like substance that can cause the cyst to expand and potentially lead to complications. These tumors are predominantly found in women, particularly those over the age of 50. While some pancreatic mucinous cystic neoplasms are benign, others have the potential to become malignant, making early diagnosis and treatment crucial.
There are two main types of mucinous cystic neoplasms: intraductal papillary mucinous neoplasms (IPMNs) and mucinous cystic neoplasms (MCNs). IPMNs are associated with the pancreatic ducts, while MCNs form in the body or tail of the pancreas. Both types share similar characteristics, such as the production of mucin and the potential for malignant transformation. Understanding the differences between these subtypes is essential for tailoring appropriate treatment plans.
Several factors contribute to the development of pancreatic mucinous cystic neoplasms, including genetic mutations, hormonal influences, and lifestyle choices. Research has shown that certain genetic syndromes, such as hereditary pancreatitis, may increase the risk of developing these tumors. Additionally, smoking and a diet high in processed foods may play a role in their formation. By identifying these risk factors, individuals can take proactive steps to reduce their likelihood of developing the condition.
How Common Are Pancreatic Mucinous Cystic Neoplasms?
Pancreatic mucinous cystic neoplasms are relatively uncommon compared to other pancreatic conditions. However, advancements in imaging technology have led to an increase in their detection, particularly during routine abdominal scans. Studies suggest that approximately 2% of the population may harbor pancreatic cysts, with mucinous cystic neoplasms accounting for a smaller subset of these cases. Despite their rarity, the potential for malignant transformation makes them a significant concern for healthcare providers and patients alike.
Can Pancreatic Mucinous Cystic Neoplasms Be Prevented?
While there is no guaranteed way to prevent pancreatic mucinous cystic neoplasms, certain lifestyle modifications can help reduce the risk. Maintaining a healthy weight, eating a balanced diet rich in fruits and vegetables, and avoiding smoking are all recommended strategies. Regular medical check-ups, especially for individuals with a family history of pancreatic conditions, can aid in early detection and management. By adopting these preventive measures, individuals can take control of their health and minimize the chances of developing this condition.
Symptoms of Pancreatic Mucinous Cystic Neoplasm
The symptoms of pancreatic mucinous cystic neoplasms can vary depending on the size, location, and stage of the tumor. In many cases, these cysts are asymptomatic and are only discovered during imaging tests performed for unrelated reasons. However, as the cyst grows, it can cause a range of symptoms that affect the digestive system and overall well-being. Common signs include:
Read also:Exploring The World Of Ed Edd N Eddy Sisters A Comprehensive Guide
- A feeling of fullness or bloating
- Abdominal pain, particularly in the upper abdomen
- Jaundice, characterized by yellowing of the skin and eyes
- Unexplained weight loss
- Nausea and vomiting
It's important to note that these symptoms can also be associated with other pancreatic conditions, making accurate diagnosis crucial. If you experience any of these symptoms, especially if they persist or worsen over time, it's advisable to consult a healthcare professional for further evaluation.
What Causes the Symptoms of Pancreatic Mucinous Cystic Neoplasm?
The symptoms of pancreatic mucinous cystic neoplasms are primarily caused by the growth and expansion of the cystic tumor. As the cyst enlarges, it can compress surrounding organs and structures, leading to discomfort and digestive issues. Additionally, the production of mucin can obstruct pancreatic ducts, resulting in impaired enzyme secretion and nutrient absorption. In some cases, the cyst may rupture or bleed, causing acute pain and other complications.
How Do Symptoms Progress Over Time?
As pancreatic mucinous cystic neoplasms grow, their symptoms tend to become more pronounced. Initially, patients may only experience mild discomfort or intermittent pain. Over time, however, the cyst can cause more severe symptoms, such as persistent abdominal pain, jaundice, and digestive disturbances. Regular monitoring and follow-up with a healthcare provider are essential for tracking the progression of symptoms and adjusting treatment plans accordingly.
Diagnosing Pancreatic Mucinous Cystic Neoplasm
Diagnosing pancreatic mucinous cystic neoplasm involves a combination of imaging tests, laboratory analyses, and clinical evaluations. Early detection is critical, as it allows for timely intervention and improved outcomes. Healthcare providers typically begin the diagnostic process by reviewing the patient's medical history and conducting a thorough physical examination. If a pancreatic cyst is suspected, additional tests may be ordered to confirm the diagnosis and determine the type of cystic neoplasm.
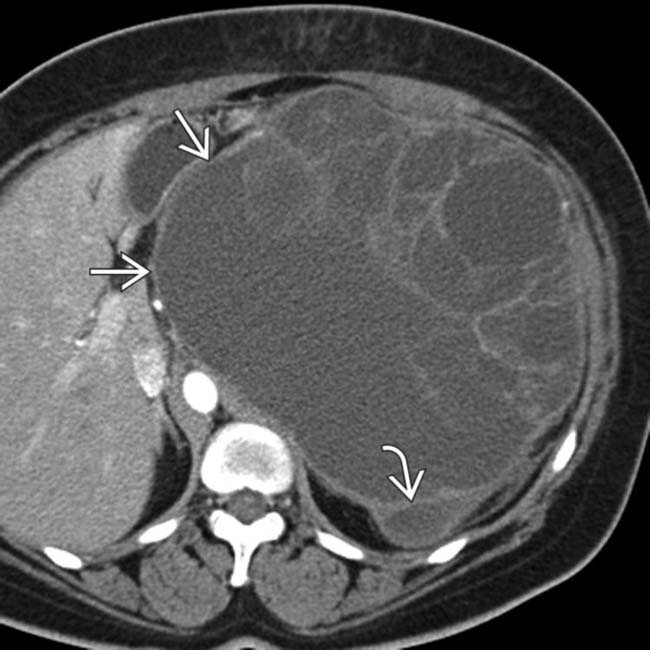
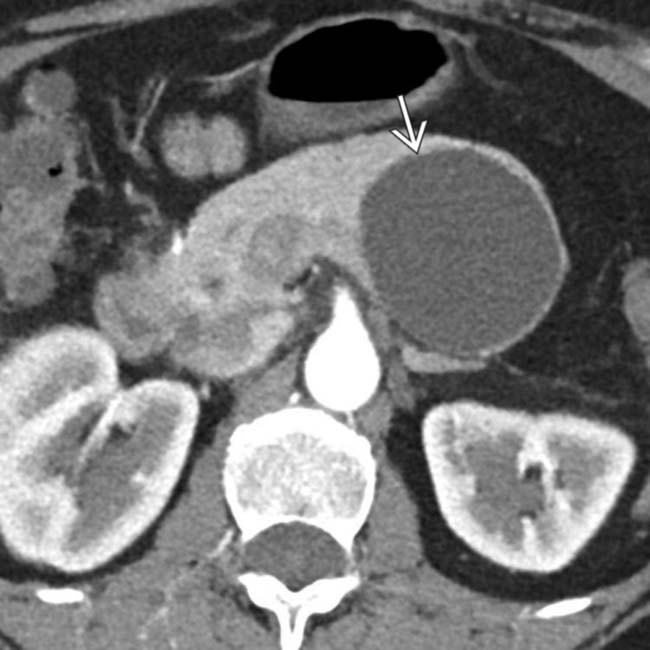
Imaging studies, such as abdominal ultrasound, computed tomography (CT), and magnetic resonance imaging (MRI), are commonly used to visualize the pancreas and identify cystic lesions. Endoscopic ultrasound (EUS) is another valuable tool that provides detailed images of the pancreas and allows for fine-needle aspiration (FNA) of the cyst for further analysis. Laboratory tests, including blood work and tumor marker assessments, can also help differentiate between benign and malignant cysts.
In some cases, genetic testing may be recommended, especially for individuals with a family history of pancreatic conditions or known genetic syndromes. This testing can provide insights into the likelihood of developing pancreatic mucinous cystic neoplasms and guide personalized treatment strategies. By utilizing a comprehensive diagnostic approach, healthcare providers can accurately diagnose pancreatic mucinous cystic neoplasms and develop effective management plans.
Treatment Options for Pancreatic Mucinous Cystic Neoplasm
The treatment of pancreatic mucinous cystic neoplasm depends on several factors, including the size, location, and potential for malignant transformation of the cyst. For small, asymptomatic cysts with a low risk of malignancy, active surveillance may be recommended. This involves regular imaging and follow-up appointments to monitor the cyst for any changes. If the cyst shows signs of growth or increased risk, surgical intervention may be necessary.
Surgical options for pancreatic mucinous cystic neoplasms include cyst resection, pancreaticoduodenectomy (Whipple procedure), and distal pancreatectomy. The choice of surgery depends on the specific characteristics of the cyst and the patient's overall health. Minimally invasive techniques, such as laparoscopic or robotic-assisted surgery, are often preferred due to their shorter recovery times and reduced complications.
In addition to surgery, other treatment modalities, such as chemotherapy and radiation therapy, may be considered for advanced cases or those with malignant transformation. These therapies aim to shrink the tumor, prevent its spread, and improve the patient's quality of life. Collaboration between a multidisciplinary team of specialists, including gastroenterologists, surgeons, and oncologists, ensures the best possible outcomes for patients with pancreatic mucinous cystic neoplasms.
Which Treatment Option Is Best for Me?
The optimal treatment option for pancreatic mucinous cystic neoplasm varies depending on individual circumstances. Factors such as the patient's age, overall health, and personal preferences play a significant role in determining the most suitable approach. Consulting with a healthcare provider who specializes in pancreatic conditions can help clarify the benefits and risks associated with each treatment option. By working closely with your medical team, you can make an informed decision that aligns with your goals and priorities.
What Are the Potential Risks of Surgery?
As with any surgical procedure, there are potential risks associated with treating pancreatic mucinous cystic neoplasms. These may include bleeding, infection, and complications related to anesthesia. In some cases, surgery may lead to temporary or permanent digestive issues, such as difficulty digesting fats or maintaining blood sugar levels. Despite these risks, the benefits of removing a potentially malignant cyst often outweigh the drawbacks. Discussing these risks with your surgeon beforehand can help alleviate concerns and ensure a smoother recovery process.
Living with Pancreatic Mucinous Cystic Neoplasm
Living with pancreatic mucinous cystic neoplasm requires a proactive approach to managing symptoms and maintaining overall well-being. Adopting a healthy lifestyle, staying informed about the condition, and maintaining open communication with healthcare providers are all essential components of effective management. Patients may find it helpful to join support groups or connect with others who have experienced similar challenges, as sharing experiences and advice can provide valuable emotional support.
Incorporating dietary changes, such as reducing fat intake and increasing fiber consumption, can aid in managing digestive symptoms and improving nutrient absorption. Regular exercise, stress management techniques, and adequate rest are also important for maintaining physical and mental health. By prioritizing self-care and adhering to recommended treatment plans, individuals with pancreatic mucinous cystic neoplasms can lead fulfilling and active lives.
Frequently Asked Questions
Is Pancreatic Mucinous Cystic Neoplasm Always Cancerous?
No, pancreatic mucinous cystic neoplasm is not always cancerous. While these cystic tumors have the potential to become malignant, many are benign or premalignant. Regular monitoring and follow-up with a healthcare provider can help determine the risk of malignant transformation and guide appropriate treatment decisions.
Can Pancreatic Mucinous Cystic Neoplasm Be Cured?
Yes, pancreatic mucinous cystic neoplasm can often be cured, especially when detected early and treated promptly. Surgical removal of the cyst is typically the most effective treatment for preventing malignant transformation. In cases where malignancy has already occurred, a combination of surgery, chemotherapy, and radiation therapy may be necessary to achieve remission.
Conclusion
Pancreatic mucinous cystic neoplasm is a complex condition that requires careful attention and management. By understanding its symptoms, diagnosis, and treatment options, individuals can take proactive steps to ensure the best possible outcomes. With advancements in medical technology and increasing awareness of pancreatic conditions, patients have more resources than ever before to manage this condition effectively. Remember, early detection and collaboration with healthcare professionals are key to overcoming the challenges posed by pancreatic mucinous cystic neoplasm.
Table of Contents
- What Is Pancreatic Mucinous Cystic Neoplasm?
- How Common Are Pancreatic Mucinous Cystic Neoplasms?
- Can Pancreatic Mucinous Cystic Neoplasms Be Prevented?
- Symptoms of Pancreatic Mucinous Cystic Neoplasm
- What Causes the Symptoms of Pancreatic Mucinous Cystic Neoplasm?
- Diagnosing Pancreatic Mucinous Cystic Neoplasm